Further link identified between autoimmunity and schizophrenia
Tokyo, Japan – Links have been reported between schizophrenia and proteins produced by the immune system that can act against one’s own body, known as autoantibodies. In a study published last month in Brain Behavior and Immunity, Japanese researchers identified autoantibodies that target a ‘synaptic adhesion protein’, neurexin 1α, in a subset of patients with schizophrenia. When injected into mice, the autoantibodies caused many schizophrenia-related changes.
What is a synaptic protein, and why might it be linked to schizophrenia? Synaptic adhesion proteins are specialized proteins that bind to create physical connections between brain cells. These connections, called synapses, allow the cells to communicate by passing molecules back and forth. Both synapses and autoimmunity are known to be associated with schizophrenia, so the research team from Tokyo Medical and Dental University (TMDU) decided to investigate autoantibodies that target synaptic proteins in patients with schizophrenia.
“In around 2% of our patient population, we identified autoantibodies against the synaptic protein neurexin 1α, which is expressed by one cell in the synapse and binds to proteins known as neuroligins on the other cell in the synapse,” says lead author of the study Hiroki Shiwaku. “Once we had identified these autoantibodies, we wanted to see if they were able to cause schizophrenia-related changes.”
To do this, the researchers isolated autoantibodies from some of the patients with schizophrenia and injected them into the cerebrospinal fluid of mice, so that the autoantibodies would travel into the brain. In these mice, the autoantibodies blocked neurexin 1α and neuroligin binding and altered some related synaptic properties. The administration of these autoantibodies also resulted in fewer synapses in the brains of mice and schizophrenia-related behaviors, such as reduced social behavior toward unfamiliar mice and reduced cognitive function.
“Together, our results strongly suggest that autoantibodies against neurexin 1α can cause schizophrenia-related changes, at least in mice,” explains Hiroki Shiwaku. “These autoantibodies may therefore represent a therapeutic target for a subset of patients with schizophrenia.”
Schizophrenia has a wide variety of both symptoms and treatment responses, and many patients have symptoms that are resistant to currently available treatment options. Therefore, the identification of possible disease-causing autoantibodies is important for improving symptom control in patients with schizophrenia. It is hoped that the results of this investigation will allow patients with autoantibodies that target neurexin 1α—all of whom were resistant to antipsychotic treatment in the present study—to better control their symptoms in the future.
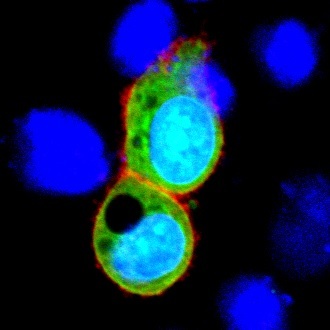
Cell-based assay to detect the anti-NRXN1 autoantibody
NRXN1 is induced only in green cells (HeLa cells). Serum from patients with anti-NRXN1 autoantibody react only to green cells (framed in red).
Summary
Journal Article
TITLE:Analyzing schizophrenia-related phenotypes in mice caused by autoantibodies against NRXN1α in schizophrenia
DOI:https://doi.org/10.1016/j.bbi.2023.03.028
Correspondence to
Hiroki Shiwaku, M.D., Ph.D., Assistant Professor
Department of Psychiatry and Behavioral Sciences,
Graduate School of Medical and Dental Sciences,
Tokyo Medical and Dental University(TMDU)
E-mail:shiwnpat(at) tmd.ac.jp
*Please change (at) in e-mail addresses to @ on sending your e-mail to contact personnels.

