"Method Identified to Boost Detection of Highly Cancerous Stem Cells"
Japanese researchers identify process to improve fluorescence detection of cancer stem cells, which are primarily responsible for brain tumor progression and recurrence after treatment
Tokyo – Photodynamic detection and therapy has recently emerged as a promising approach for diagnosing and treating cancer. With this process, patients are given a chemical metabolized specifically in tumor cells so that it becomes fluorescent, allowing visual identification and surgical removal of the tumor.
Complete removal of all cancerous cells is crucial, as any residual cells can cause tumor recurrence. However, tumors are made up of a variety of different cell types, and it has been unclear whether photodynamic detection identifies all of them. Cancer stem cells, a type of self-renewing cell found in tumors, are of particular interest because they are the main cell type responsible for tumor progression and for resistance to chemotherapy and radiotherapy, and therefore a major cause of tumor recurrence after treatment. Assessing and optimizing photodynamic detection for cancer stem cell detection is vital to the approach’s success.
Tokyo – Photodynamic detection and therapy has recently emerged as a promising approach for diagnosing and treating cancer. With this process, patients are given a chemical metabolized specifically in tumor cells so that it becomes fluorescent, allowing visual identification and surgical removal of the tumor.
Complete removal of all cancerous cells is crucial, as any residual cells can cause tumor recurrence. However, tumors are made up of a variety of different cell types, and it has been unclear whether photodynamic detection identifies all of them. Cancer stem cells, a type of self-renewing cell found in tumors, are of particular interest because they are the main cell type responsible for tumor progression and for resistance to chemotherapy and radiotherapy, and therefore a major cause of tumor recurrence after treatment. Assessing and optimizing photodynamic detection for cancer stem cell detection is vital to the approach’s success.
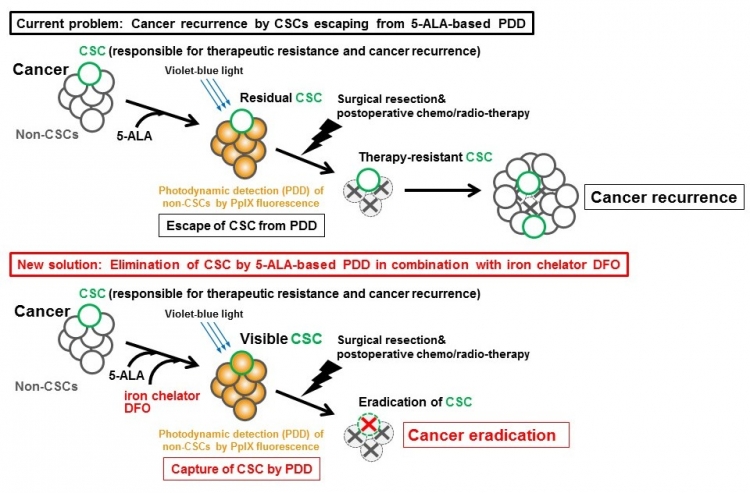
Fig : A current limitation and a new strategy to detect CSCs for cancer eradication
Cancer stem cells (CSCs) escape from 5-aminolevulinic acid (5-ALA)-based photodynamic detection (PDD) (upper panel). An iron chelator deferoxamine (DFO) enhances accumulation in CSCs of PpIX from 5-ALA, which will facilitate the elimination of CSCs for cancer eradication.
In a new study published in Scientific Reports, Tokyo Medical and Dental University (TMDU)-led researchers investigated photodynamic detection of cancer stem cells in a glioma cell line, a model of a highly aggressive type of brain cancer. They identified a subpopulation of glioma stem cells, which, unlike most glioma cells, did not accumulate substantial amounts of fluorescent product during photodynamic detection. When transplanted into immunosuppressed mice, these low-fluorescence stem cells rapidly formed tumors, whereas high-fluorescence stem cells did not.
“This is a clear problem for photodynamic detection,” corresponding author Tetsuya Taga says. “The cells that escape detection are the ones that, if not removed, are the most likely to result in treatment failing and a tumor recurring. By increasing fluorescence in these cells, we could substantially improve the success of fluorescence detection and tumor removal.”
The researchers went on to investigate possible mechanisms for, and solutions to, low fluorescence levels. Iron is required to break down the fluorescent material in cells, so they explored chelating iron (binding it to prevent it from participating in this process).
“We were able to boost fluorescence accumulation in the highly tumorigenic low-fluorescence glioma stem cell subpopulation using a clinically approved iron chelator,” co-corresponding author Kouichi Tabu says. “This is particularly exciting because it means this new method has potential to rapidly translate to clinical practice.”
Further investigation of the metabolic pathway that breaks down the fluorescent material revealed a gene, heme oxygenase-1 (HO-1), that may be responsible for the differences in fluorescence. Targeting HO-1 is therefore another potential approach to improving photodynamic detection in human glial cell cancers.
The article, “Enhancement of 5-aminolevulinic acid-based fluorescence detection of side population-defined glioma stem cells by iron chelation” was published in Scientific Reports at DOI:10.1038/srep42070
“This is a clear problem for photodynamic detection,” corresponding author Tetsuya Taga says. “The cells that escape detection are the ones that, if not removed, are the most likely to result in treatment failing and a tumor recurring. By increasing fluorescence in these cells, we could substantially improve the success of fluorescence detection and tumor removal.”
The researchers went on to investigate possible mechanisms for, and solutions to, low fluorescence levels. Iron is required to break down the fluorescent material in cells, so they explored chelating iron (binding it to prevent it from participating in this process).
“We were able to boost fluorescence accumulation in the highly tumorigenic low-fluorescence glioma stem cell subpopulation using a clinically approved iron chelator,” co-corresponding author Kouichi Tabu says. “This is particularly exciting because it means this new method has potential to rapidly translate to clinical practice.”
Further investigation of the metabolic pathway that breaks down the fluorescent material revealed a gene, heme oxygenase-1 (HO-1), that may be responsible for the differences in fluorescence. Targeting HO-1 is therefore another potential approach to improving photodynamic detection in human glial cell cancers.
The article, “Enhancement of 5-aminolevulinic acid-based fluorescence detection of side population-defined glioma stem cells by iron chelation” was published in Scientific Reports at DOI:10.1038/srep42070
Summary:
Tokyo Medical and Dental University (TMDU)-led researchers discovered a subpopulation of highly cancerous stem cells in a brain cancer cell line. The cells are not identified by standard tumor cell fluorescence detection methods. By investigating the pathways involved in breaking down the fluorescent labelling material, the research team discovered that by reducing the availability of iron they could enhance fluorescence detection of these cells.
Correspondence to:
Tetsuya Taga, Ph.D., Professor and Kouichi Tabu, Ph.D., Assistant Professor
Department of Stem Cell Regulation, Medical Research Institute,
Tokyo Medical and Dental University (TMDU)
M&D tower 24th Floor, 1-5-45, Yushima, Bunkyo-ku, Tokyo, 113-8510, Japan
E-mail: taga.scr(at)mri.tmd.ac.jp (TT) and k-tabu.scr(at)mri.tmd.ac.jp (KT)
*Please change (at) in the e-mail addresses to @ when sending correspondence.
Department of Stem Cell Regulation, Medical Research Institute,
Tokyo Medical and Dental University (TMDU)
M&D tower 24th Floor, 1-5-45, Yushima, Bunkyo-ku, Tokyo, 113-8510, Japan
E-mail: taga.scr(at)mri.tmd.ac.jp (TT) and k-tabu.scr(at)mri.tmd.ac.jp (KT)
*Please change (at) in the e-mail addresses to @ when sending correspondence.

