How poor oral hygiene may result in metabolic syndrome
Researchers from Tokyo Medical and Dental University (TMDU) identify a novel mechanism by which periodontal disease may cause diabetes
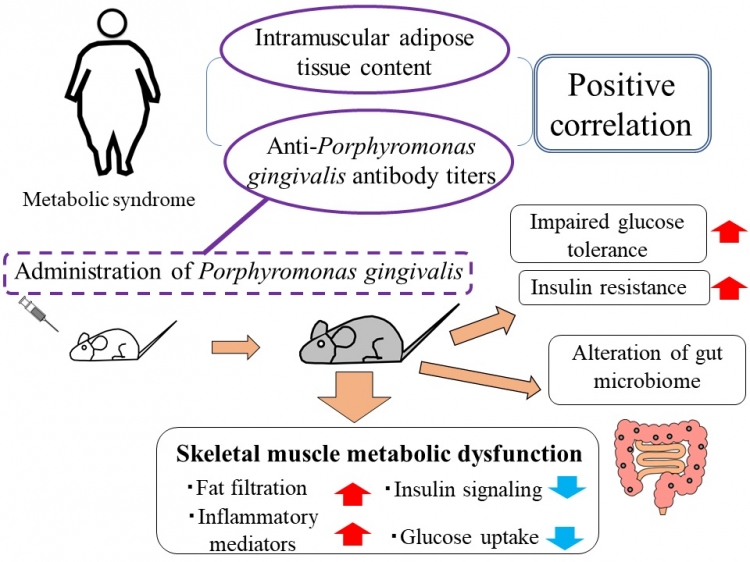
Tokyo, Japan – Periodontal or gum disease is known to be a significant risk factor of metabolic syndrome, a group of conditions increasing the risk for heart disease and diabetes. In a new study, researchers from Tokyo Medical and Dental University (TMDU) discovered that infection with Porphyromonas gingivalis, the bacterium causing periodontal disease, causes skeletal muscle metabolic dysfunction, the precursor to metabolic syndrome, by altering the composition of the gut microbiome.
Periodontal bacteria have long been known to cause inflammation within the oral cavity, but also systemically increase inflammatory mediators. As a result, sustained infection with periodontal bacteria can lead to increases in body weight and lead to increased insulin resistance, a hallmark of type 2 diabetes. The function of insulin is to help shuttle glucose from the blood into tissues, most importantly to skeletal muscle, where one quarter of all glucose in stored. Unsurprisingly, insulin resistance plays a key role in the development of metabolic syndrome, a group of conditions including obesity, altered lipid metabolism, high blood pressure, high blood glucose levels, and systemic inflammation. Although skeletal muscle plays a key role in decreasing blood glucose levels, a direct connection between periodontal bacterial infection and the metabolic function of skeletal muscle has not been established yet.
“Metabolic syndrome has become a widespread health problem in the developed world,” says first author of the study Kazuki Watanabe. “The goal of our study was to investigate how periodontal bacterial infection might lead to metabolic alterations in skeletal muscle and thus to the development of metabolic syndrome.”
To achieve their goal, the researchers first investigated antibody titers to Porphyromonas gingivalis in the blood of patients with metabolic syndrome and found a positive correlation between antibody titers and increased insulin resistance. These results showed that patients with metabolic syndrome were likely to have undergone infection with Porphyromonas gingivalis and thus have mounted an immune response yielding antibodies against the germ. To understand the mechanism behind the clinical observation, the researchers then turned to an animal model. When they gave mice that were fed a high-fat diet (a pre-requisite to developing metabolic syndrome) Porphyromonas gingivalis by mouth, the mice developed increased insulin resistance, and fat infiltration and lower glucose uptake in the skeletal muscle compared with mice that did not receive the bacteria.
But how was this bacterium capable of causing systemic inflammation and metabolic syndrome? To answer this question, the researchers focused on the gut microbiome, the network of bacteria present in the gut and with which the organism co-exists symbiotically. Intriguingly, the researchers found that in mice administered with Porphyromonas gingivalis the gut microbiome was significantly altered, which might decrease insulin sensitivity.
“These are striking results that provide a mechanism underlying the relationship between infection with the periodontal bacterium Porphyromonas gingivalis and the development of metabolic syndrome and metabolic dysfunction in skeletal muscle,” says corresponding author of the study Professor Sayaka Katagiri.
Tokyo, Japan – Periodontal or gum disease is known to be a significant risk factor of metabolic syndrome, a group of conditions increasing the risk for heart disease and diabetes. In a new study, researchers from Tokyo Medical and Dental University (TMDU) discovered that infection with Porphyromonas gingivalis, the bacterium causing periodontal disease, causes skeletal muscle metabolic dysfunction, the precursor to metabolic syndrome, by altering the composition of the gut microbiome.
Periodontal bacteria have long been known to cause inflammation within the oral cavity, but also systemically increase inflammatory mediators. As a result, sustained infection with periodontal bacteria can lead to increases in body weight and lead to increased insulin resistance, a hallmark of type 2 diabetes. The function of insulin is to help shuttle glucose from the blood into tissues, most importantly to skeletal muscle, where one quarter of all glucose in stored. Unsurprisingly, insulin resistance plays a key role in the development of metabolic syndrome, a group of conditions including obesity, altered lipid metabolism, high blood pressure, high blood glucose levels, and systemic inflammation. Although skeletal muscle plays a key role in decreasing blood glucose levels, a direct connection between periodontal bacterial infection and the metabolic function of skeletal muscle has not been established yet.
“Metabolic syndrome has become a widespread health problem in the developed world,” says first author of the study Kazuki Watanabe. “The goal of our study was to investigate how periodontal bacterial infection might lead to metabolic alterations in skeletal muscle and thus to the development of metabolic syndrome.”
To achieve their goal, the researchers first investigated antibody titers to Porphyromonas gingivalis in the blood of patients with metabolic syndrome and found a positive correlation between antibody titers and increased insulin resistance. These results showed that patients with metabolic syndrome were likely to have undergone infection with Porphyromonas gingivalis and thus have mounted an immune response yielding antibodies against the germ. To understand the mechanism behind the clinical observation, the researchers then turned to an animal model. When they gave mice that were fed a high-fat diet (a pre-requisite to developing metabolic syndrome) Porphyromonas gingivalis by mouth, the mice developed increased insulin resistance, and fat infiltration and lower glucose uptake in the skeletal muscle compared with mice that did not receive the bacteria.
But how was this bacterium capable of causing systemic inflammation and metabolic syndrome? To answer this question, the researchers focused on the gut microbiome, the network of bacteria present in the gut and with which the organism co-exists symbiotically. Intriguingly, the researchers found that in mice administered with Porphyromonas gingivalis the gut microbiome was significantly altered, which might decrease insulin sensitivity.
“These are striking results that provide a mechanism underlying the relationship between infection with the periodontal bacterium Porphyromonas gingivalis and the development of metabolic syndrome and metabolic dysfunction in skeletal muscle,” says corresponding author of the study Professor Sayaka Katagiri.
Summary of the study
Anti-Porphyromonas gingivalis antibody titers positively correlated with intramuscular adipose tissue content in metabolic syndrome patients. Administration of P. gingivalis impaired glucose tolerance and insulin resistance, altered the gut microbiome. Skeletal muscle of recipients of P. gingivalis exhibited fat infiltration and lower glucose uptake with higher inflammatory mediators and lower insulin signaling.
###
The article, “Porphyromonas gingivalis impairs glucose uptake in skeletal muscle associated with altering gut microbiota” has been published in The FASEB Journal at DOI: 10.1096/fj.202001158R
The article, “Porphyromonas gingivalis impairs glucose uptake in skeletal muscle associated with altering gut microbiota” has been published in The FASEB Journal at DOI: 10.1096/fj.202001158R
Summary
Researchers from TMDU identified a novel mechanism by which periodontal disease may cause metabolic syndrome. By studying patients with metabolic syndrome, the researchers demonstrated high antibody titers against Porphyromonas gingivalis, the bacterium causing periodontal disease. In a mouse model, the researchers then showed that infection with this bacterium causes systemic insulin resistance and metabolic dysfunction in skeletal muscle by altering the gut microbiome. This study shows the effect periodontal disease can have on the entire body.
Correspondence to
Sayaka KATAGIRI,Junior Associate Professor
Department of Periodontology,
Graduate School of Medical and Dental Sciences,
Tokyo Medical and Dental University (TMDU),
E-mail:katagiri.peri(at)tmd.ac.jp
*Please change (at) in e-mail addresses to @ on sending your e-mail to contact personnels.
Department of Periodontology,
Graduate School of Medical and Dental Sciences,
Tokyo Medical and Dental University (TMDU),
E-mail:katagiri.peri(at)tmd.ac.jp
*Please change (at) in e-mail addresses to @ on sending your e-mail to contact personnels.

