Light stimulation makes bones heavier
Researchers from Tokyo Medical and Dental University (TMDU) show that laser irradiation inhibits expression of the osteogenesis inhibitor protein sclerostin without causing inflammation, providing a potential therapeutic option for osteoporosis
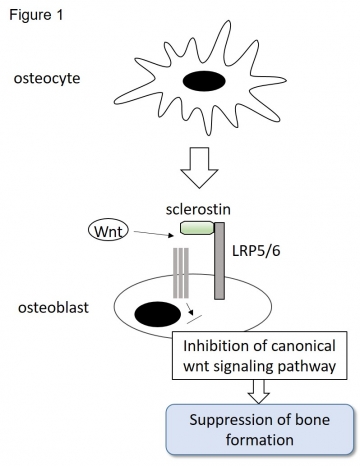
Tokyo, Japan – Osteoporosis is a disease in which bone loses mass as a result of age or other influences. This weakening is the leading cause of fractures in the elderly, often after trivial injuries, and makes treating these “pathological fractures” a challenge. Bone health is a dynamic process of continual remodeling controlled by multiple factors. Sclerostin, a glycoprotein coded by the gene SOST, is produced by bone cells and suppresses bone formation. Now, researchers at Tokyo Medical and Dental University (TMDU) have shown that laser irradiation, by inhibiting sclerostin expression without inducing inflammation, shows promise as a new treatment modality for osteoporosis.
Lasers have been used in medical and dental practice for their beneficial photo-biomodulation effects on tissue healing. The benefits of low-level laser therapy are now gaining increased attention in spheres of medicine and dentistry that require enhanced bone regeneration.
The team knew that in periodontal surgery, bone that underwent controlled destruction using a specific type of laser known as an Er:YAG laser healed faster than bone subjected to conventional bur drilling. Thus, they wondered whether Er:YAG laser irradiation modified SOST expression in bone. “We set out to compare comprehensive and sequential gene expression and biological healing responses in laser-ablated, bur-drilled, and untreated bone, as well as investigating the bio-stimulation effect of an Er:YAG laser on osteogenic cells,” explains Yujin Ohsugi, lead author.
Tokyo, Japan – Osteoporosis is a disease in which bone loses mass as a result of age or other influences. This weakening is the leading cause of fractures in the elderly, often after trivial injuries, and makes treating these “pathological fractures” a challenge. Bone health is a dynamic process of continual remodeling controlled by multiple factors. Sclerostin, a glycoprotein coded by the gene SOST, is produced by bone cells and suppresses bone formation. Now, researchers at Tokyo Medical and Dental University (TMDU) have shown that laser irradiation, by inhibiting sclerostin expression without inducing inflammation, shows promise as a new treatment modality for osteoporosis.
Lasers have been used in medical and dental practice for their beneficial photo-biomodulation effects on tissue healing. The benefits of low-level laser therapy are now gaining increased attention in spheres of medicine and dentistry that require enhanced bone regeneration.
The team knew that in periodontal surgery, bone that underwent controlled destruction using a specific type of laser known as an Er:YAG laser healed faster than bone subjected to conventional bur drilling. Thus, they wondered whether Er:YAG laser irradiation modified SOST expression in bone. “We set out to compare comprehensive and sequential gene expression and biological healing responses in laser-ablated, bur-drilled, and untreated bone, as well as investigating the bio-stimulation effect of an Er:YAG laser on osteogenic cells,” explains Yujin Ohsugi, lead author.
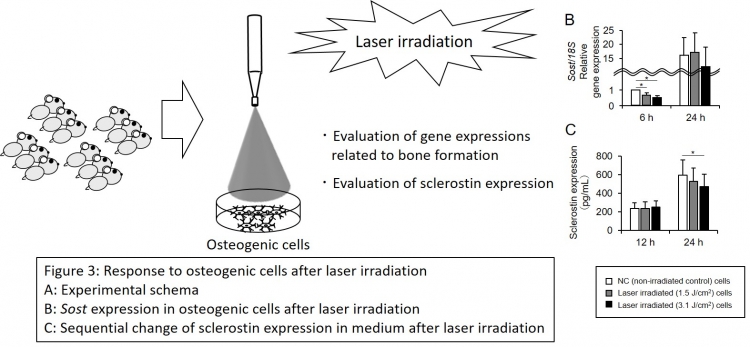
Using microarray analysis, the researchers first studied gene expression patterns in rat skull bones during healing at 6, 24, and 72 hours after drilling or laser treatment. Immunohistochemical analysis at 1 day was performed to detect sclerostin expression. Additionally, oseteogenic cell cultures were irradiated in vitro and assessed for cell death and sclerostin concentration.
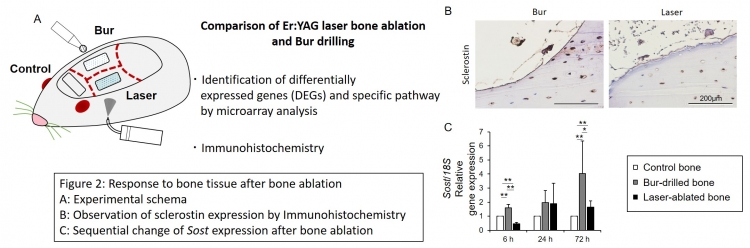
“We confirmed decreased sclerostin expression after laser irradiation both in vivo and in vitro,” affirms Sayaka Katagiri, corresponding author. “Interestingly, sequential microarray analysis revealed a clear distinction in the gene expression pattern between bur-drilled and laser-ablated bones at 24 hours, with the former alone showing enriched inflammation-related pathways. Significantly, at 6 hours following laser ablation, the Hippo signaling pathway that limits tissue overgrowth was enriched but inflammation-related pathways remained unaffected, suggesting that laser irradiation worked thorough mechanical bio-stimulation.”
The finding that mechanical stimulation of laser irradiation inhibits the pathways that suppress bone regeneration without provoking inflammation may aid development of laser-based therapeutic methods. Such methods might be used in treatments for osteoporosis and to induce or promote bone regeneration in medical and dental procedures.
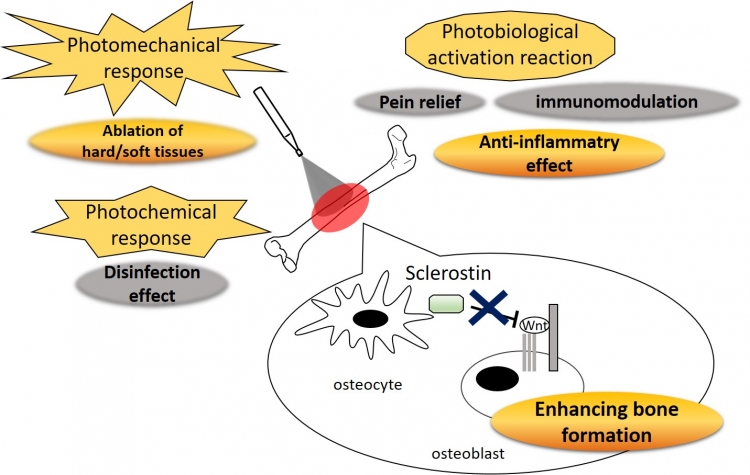
The effect of Er:YAG laser irradiation on the bone tissue.
Laser irradiation causes photomechanical response, photobiological activation reaction, and photochemical response in the various tissues and cells. Downregulation of Sost expression in the bone tissue was observed after Er:YAG laser bone ablation. Because sclerostin (coded by Sost) suppressed bone formation by inhibiting canonical Wnt signaling pathway, there is a possibility that Er:YAG laser irradiation to the bone enhances bone formation.
Laser irradiation causes photomechanical response, photobiological activation reaction, and photochemical response in the various tissues and cells. Downregulation of Sost expression in the bone tissue was observed after Er:YAG laser bone ablation. Because sclerostin (coded by Sost) suppressed bone formation by inhibiting canonical Wnt signaling pathway, there is a possibility that Er:YAG laser irradiation to the bone enhances bone formation.
###
The article, “Laser irradiation decreases sclerostin expression in bone and osteogenic cells” was published in The FASEB Journal at DOI: 10.1096/fj.202001032R.
The article, “Laser irradiation decreases sclerostin expression in bone and osteogenic cells” was published in The FASEB Journal at DOI: 10.1096/fj.202001032R.
Summary
Tokyo Medical and Dental University (TMDU) researchers showed that laser ablation of bone inhibits expression of the osteogenesis inhibitor protein sclerostin without causing inflammation, unlike the conventional bur-drilling technique. Further investigations confirmed that this beneficial bio-stimulation works by inducing mechanical stress. These findings help advance research into the treatment of osteoporosis as well as specific enhancement of bone regrowth in orthopedic and dental surgery.
Correspondence to
Ohsugi Yujin, Dental Resident
E-mail: ohsugi.peri(at)tmd.ac.jp
Sayaka Katagiri, Junior Associate Professor
E-mail: kataperi(at)tmd.ac.jp
Aoki Akira, Professer
E-mail: aoperi(at)tmd.ac.jp
Department of Periodontology
Graduate School of Medical and Dental Sciences
Tokyo Medical and Dental University(TMDU)
*Please change (at) in e-mail addresses to @ on sending your e-mail to contact personnels.
E-mail: ohsugi.peri(at)tmd.ac.jp
Sayaka Katagiri, Junior Associate Professor
E-mail: kataperi(at)tmd.ac.jp
Aoki Akira, Professer
E-mail: aoperi(at)tmd.ac.jp
Department of Periodontology
Graduate School of Medical and Dental Sciences
Tokyo Medical and Dental University(TMDU)
*Please change (at) in e-mail addresses to @ on sending your e-mail to contact personnels.

