Graduate Course
Our PhD program provides advanced training of researchers in the field of prosthodontics.
Welcome to our Graduate Course
Removable Partial Prosthodontics,
Department of Masticatory Function Rehabilitation,
Division of Oral Health Sciences,
Graduate School,Tokyo Medical and Dental University,
1-5-45, Yushima, Bunkyo-ku, Tokyo 113-8549, Japan
(Location: Building #5 in the campus map, 11th Floor
Contact for general information: Dr. Junichiro Wada, Senior Associate, DDS, PhD
Contact for program: Dr. Noriyuki Wakabayashi, Professor, DDS, PhD
Admission Inquiry: Dr. Mai Murase, Assistant Professor, DDS, PhD
Department of Masticatory Function Rehabilitation,
Division of Oral Health Sciences,
Graduate School,Tokyo Medical and Dental University,
1-5-45, Yushima, Bunkyo-ku, Tokyo 113-8549, Japan
(Location: Building #5 in the campus map, 11th Floor
Contact for general information: Dr. Junichiro Wada, Senior Associate, DDS, PhD
Contact for program: Dr. Noriyuki Wakabayashi, Professor, DDS, PhD
Admission Inquiry: Dr. Mai Murase, Assistant Professor, DDS, PhD
Summary in English
The Department of Removable Partial Prosthodontics specializes in removable partial denture treatment, which is one of the major disciplines of clinical dentistry. The department has taken the baton from the First Department of Prosthodontics and the Department of Masticatory Function Rehabilitation.
Our objectives are to enhance the art and science of removable prosthodontics for the management of various oral conditions associated with tooth loss, from a single missing tooth to a single remaining tooth, in the maxillary and/or mandibular arch.
Research
1. Treatment Planning, Treatment and Evaluation in Prosthodontics
2. Design Optimization of Prosthodontic Biomaterials
3. Biological Evaluation of Oral Tissues in Prosthodontic Patients
4. Educational Development in Prosthodontics
Education
This department offers a variety of educational courses pertaining to the specialized clinical management of tooth loss, primarily for undergraduate students at the School of Dentistry. The courses include lectures, tutorials, hands-on sessions, clinical simulations, and clinical internship instructions.
The ability to perform clinical operations on patients with tooth loss, including the skills required for medical interviews, oral examinations, diagnosis, decision making, impression making, bite registration, denture design and technology, and denture delivery and maintenance, is essential for clinical dental professionals. The objectives of our courses are to provide learning and training in contemporary removable prosthodontics and enhance the knowledge and skills of students to help them develop and flourish in their future career as dental and oral health professionals.
Clinical Activity
All faculty members of the Department of Advanced Prosthodontics are assigned to treat patients at the Prosthodontics department in the Dental Hospital of the Tokyo Medical and Dental University. While the rate of tooth retention has increased in comparison with previously reported rates, the number of patients in need of a removable partial denture has increased. Our specialists primarily work on advanced cases that are referred from other departments and outside the hospital. The departmental mission also includes the development and application of new prosthodontic materials, their clinical trial, and the spread of novel and inventive knowledge to the community.
Specialty in Practice
The department specializes in prosthodontics and aims to restore missing teeth and associated oral tissues; improve physiological functions such as occlusion, mastication, swallowing, and speech; maintain normal oral sensation; and restore the original appearance of individual patients.
Treatment modalities, materials, and denture design are all based on the case history and chief complaint of the patients. The ultimate goal is to improve the oral health-related quality of life of patients.
Our objectives are to enhance the art and science of removable prosthodontics for the management of various oral conditions associated with tooth loss, from a single missing tooth to a single remaining tooth, in the maxillary and/or mandibular arch.
Research
1. Treatment Planning, Treatment and Evaluation in Prosthodontics
2. Design Optimization of Prosthodontic Biomaterials
3. Biological Evaluation of Oral Tissues in Prosthodontic Patients
4. Educational Development in Prosthodontics
Education
This department offers a variety of educational courses pertaining to the specialized clinical management of tooth loss, primarily for undergraduate students at the School of Dentistry. The courses include lectures, tutorials, hands-on sessions, clinical simulations, and clinical internship instructions.
The ability to perform clinical operations on patients with tooth loss, including the skills required for medical interviews, oral examinations, diagnosis, decision making, impression making, bite registration, denture design and technology, and denture delivery and maintenance, is essential for clinical dental professionals. The objectives of our courses are to provide learning and training in contemporary removable prosthodontics and enhance the knowledge and skills of students to help them develop and flourish in their future career as dental and oral health professionals.
Clinical Activity
All faculty members of the Department of Advanced Prosthodontics are assigned to treat patients at the Prosthodontics department in the Dental Hospital of the Tokyo Medical and Dental University. While the rate of tooth retention has increased in comparison with previously reported rates, the number of patients in need of a removable partial denture has increased. Our specialists primarily work on advanced cases that are referred from other departments and outside the hospital. The departmental mission also includes the development and application of new prosthodontic materials, their clinical trial, and the spread of novel and inventive knowledge to the community.
Specialty in Practice
The department specializes in prosthodontics and aims to restore missing teeth and associated oral tissues; improve physiological functions such as occlusion, mastication, swallowing, and speech; maintain normal oral sensation; and restore the original appearance of individual patients.
Treatment modalities, materials, and denture design are all based on the case history and chief complaint of the patients. The ultimate goal is to improve the oral health-related quality of life of patients.
Program Objectives

The PhD Program in Advanced Prosthodontics provides advanced training in research and science for postgraduate dentists who may be concurrently enrolled in specialty programs. The program objectives are to provide training in modern prosthodontic research methods and equip students with the ability to critically analyze research and clinical literature. This training will prepare dental graduates for clinical faculty positions and enhance opportunities for careers as specialists in prosthodontic practice.
Research
Function and Physiology in Partial Denture Wearers
Evaluation of masticatory function and oral health reported QoL (OHRQoL) in denture wearers
We developed a new method for evaluating masticatory function using two-color wax cube. We also investigated the effect of prosthetic treatment with removable dentures improving masticatory ability and OHRQoL. We determined the minimal clinically important difference of OHRQoL in removable partial dentures. Further, we examine the responsiveness of chewing tests following removable partial denture treatment.
(principal researcher:Kenji Fueki)
We developed a new method for evaluating masticatory function using two-color wax cube. We also investigated the effect of prosthetic treatment with removable dentures improving masticatory ability and OHRQoL. We determined the minimal clinically important difference of OHRQoL in removable partial dentures. Further, we examine the responsiveness of chewing tests following removable partial denture treatment.
(principal researcher:Kenji Fueki)
Evaluation of brain activity change in response to a new oral environment
Some patients have difficulty habituating to using removable dentures. We investigated adaptive chewing-related brain activity changes in response to a new oral environment by functional magnetic resonance imaging.
(principal researcher:Yuka Inamochi)
Some patients have difficulty habituating to using removable dentures. We investigated adaptive chewing-related brain activity changes in response to a new oral environment by functional magnetic resonance imaging.
(principal researcher:Yuka Inamochi)
Splinting effect of removable partial denture on periodontally weakened remaining teeth
In partially edentulous patients with severe periodontal disease, remaining teeth are at higher risk of future tooth loss. Generally, it is recommended to remove remaining teeth with poor prognosis before making definitive dentures. However, extraction of teeth is physically and psychically undesirable for elders or patients with severe systemic disease. Removable partial denture (RPD) can be designed to splint and protect weakened remaining teeth including abutments. We have been evaluated the splinting effect of RPD on remaining teeth in laboratory study and clinical trial.
(principal researcher:Junichiro Wada)
In partially edentulous patients with severe periodontal disease, remaining teeth are at higher risk of future tooth loss. Generally, it is recommended to remove remaining teeth with poor prognosis before making definitive dentures. However, extraction of teeth is physically and psychically undesirable for elders or patients with severe systemic disease. Removable partial denture (RPD) can be designed to splint and protect weakened remaining teeth including abutments. We have been evaluated the splinting effect of RPD on remaining teeth in laboratory study and clinical trial.
(principal researcher:Junichiro Wada)
Optimization of Partial Denture Design based on Stress Analysis.
Optimization of the shape of thermoplastic resin clasp for RPD
Denture fracture is one of the factors that prevent the longevity of treatment in removable partial dentures. Improvement of fracture resistance of acrylic denture base, either for conventional or for implant-supported dentures, contributes the success of prosthetic treatments in terms of safety, longevity, and patient satisfaction of removable prosthodontics. Analysis of the fracture mechanisms based on the stress analysis is absolutely necessary when materials and components of removable partial dentures are changed.
We aim to optimize the design of removable partial dentures with excellent durability and low biotoxicity by analyzing simulations (FEM) combined with basic experiments.
(principal researcher: Natsuko Murakami)
Denture fracture is one of the factors that prevent the longevity of treatment in removable partial dentures. Improvement of fracture resistance of acrylic denture base, either for conventional or for implant-supported dentures, contributes the success of prosthetic treatments in terms of safety, longevity, and patient satisfaction of removable prosthodontics. Analysis of the fracture mechanisms based on the stress analysis is absolutely necessary when materials and components of removable partial dentures are changed.
We aim to optimize the design of removable partial dentures with excellent durability and low biotoxicity by analyzing simulations (FEM) combined with basic experiments.
(principal researcher: Natsuko Murakami)
Investigation of the materials and devices associated with prosthodontic treatment
Investigation of implant-use titanium-zirconium alloy
The main contribution of this paper is an investigation of the biocompatibility of titanium-zirconium (Ti-Zr) alloy, evaluating its corrosion resistance to better understand whether there is an optimal range or value for the Zr proportion in the alloy. We ultimately found that a Zr proportion of less than 50% would offer an ideal level of corrosion resistance for clinical applications. This contribution is theoretically and practically relevant becauseTi-Zr alloy has been investigated as an alternative to commercially pure titanium.
(principal researcher: Takeshi Ueno)
The main contribution of this paper is an investigation of the biocompatibility of titanium-zirconium (Ti-Zr) alloy, evaluating its corrosion resistance to better understand whether there is an optimal range or value for the Zr proportion in the alloy. We ultimately found that a Zr proportion of less than 50% would offer an ideal level of corrosion resistance for clinical applications. This contribution is theoretically and practically relevant becauseTi-Zr alloy has been investigated as an alternative to commercially pure titanium.
(principal researcher: Takeshi Ueno)
Surface modification of titanium implant surfaces
A chance exists for any type of cells to attach onto titanium implant surfaces. Furthermore, as carbon adsorption on titanium has been reported to be inevitable, this study examined the negative/positive biological reaction of osteoblasts and fibroblasts on carbon-deposited titanium surfaces. Notably, factors such as cell attachment, spreading, and expression of differentiation markers decreased in osteoblasts but increased in fibroblasts upon increasing carbon deposition. These findings suggest that the presence of carbon on the titanium surface would be detrimental to bone formation but might encourage connective tissue formation and wound healing. Thus, our results may inform future studies related to the optimization or tailoring of dental implants.
(principal researcher: Takeshi Ueno)
A chance exists for any type of cells to attach onto titanium implant surfaces. Furthermore, as carbon adsorption on titanium has been reported to be inevitable, this study examined the negative/positive biological reaction of osteoblasts and fibroblasts on carbon-deposited titanium surfaces. Notably, factors such as cell attachment, spreading, and expression of differentiation markers decreased in osteoblasts but increased in fibroblasts upon increasing carbon deposition. These findings suggest that the presence of carbon on the titanium surface would be detrimental to bone formation but might encourage connective tissue formation and wound healing. Thus, our results may inform future studies related to the optimization or tailoring of dental implants.
(principal researcher: Takeshi Ueno)
Investigation of a new dental prosthesis manufacturing process
Most of the metal structures used in dentistry are manufactured by the casting method. However, the procedure in conventional dental casting method is complicated, and the quality of the product depends on the skill of the operators. Therefore, a new manufacturing process for dental prosthesis is required. The application of selective laser melting process (SLM), one of the additive manufacturing, has been in the spotlight. We have been focusing on improving the mechanical properties, corrosion resistance, fatigue strength and compatibility of cobalt chromium alloys produced by SLM.
(principal researcher:Atsushi Takaichi)
Most of the metal structures used in dentistry are manufactured by the casting method. However, the procedure in conventional dental casting method is complicated, and the quality of the product depends on the skill of the operators. Therefore, a new manufacturing process for dental prosthesis is required. The application of selective laser melting process (SLM), one of the additive manufacturing, has been in the spotlight. We have been focusing on improving the mechanical properties, corrosion resistance, fatigue strength and compatibility of cobalt chromium alloys produced by SLM.
(principal researcher:Atsushi Takaichi)
Investigation of various stomatognathic problems associated with prosthodontic treatment
Prosthodontic treatments could be influenced by various factors, such as the condition of the remaining teeth and the alveolar ridge, the muscles of mastication and temporomandibular joints, biting force, age, sex, and systemic diseases such as diabetes. Diabetes is known in association with periodontitis, therefore it is possible that the diabetes affects the periodontal tissue of abutment teeth wearing removable partial dentures. Our department is planning a clinical study to clarify the effect of presence or absence of diabetes on the abutment tooth in collaboration with the department of periodontology.
Investigation of new ridge preservation materials for improving prosthodontic outcome
The reduction of the alveolar ridge volume often causes masticatory inefficiency and aesthetic impediment, which may further become a negative prognostic factor in subsequent prosthodontic treatment such as removable dentures and dental implants. Thus, we aim to be looking for a new bone formation peptide for preservation of alveolar residual ridge resorption.
(principal researcher:Yuki Arai)
The reduction of the alveolar ridge volume often causes masticatory inefficiency and aesthetic impediment, which may further become a negative prognostic factor in subsequent prosthodontic treatment such as removable dentures and dental implants. Thus, we aim to be looking for a new bone formation peptide for preservation of alveolar residual ridge resorption.
(principal researcher:Yuki Arai)
Is oral dryness associated with oral pain sensitivity in removable denture wearers?
Dry mouth is associated with not only caries and periodontal disease but also functional disorders such as chewing and swallowing and pain in the oral mucosa. For the patients using removable partial dentures, the pain caused by the denture on the mucous of the alveolar ridge is a very serious problem. We evaluated the relationship between dry mouth and the tenderness threshold of the oral mucosa.
(principal researcher:Kenji Fueki)
Dry mouth is associated with not only caries and periodontal disease but also functional disorders such as chewing and swallowing and pain in the oral mucosa. For the patients using removable partial dentures, the pain caused by the denture on the mucous of the alveolar ridge is a very serious problem. We evaluated the relationship between dry mouth and the tenderness threshold of the oral mucosa.
(principal researcher:Kenji Fueki)
Lectures concerning Removable Partial Prosthodontics (Lecture code: 8181)
●Aims/outline:
Professor and associate professors of Removable Partial Prosthodontics provides lectures on their specialty research areas in Prosthodontics. Following lecture titles outline the content of this special course; "Two points of research view for tooth loss", "Clinical evaluation of chewing ablity", "Load map to clinical research design", "Biomaterials research in Prosthodontics", "Introduction to stress analysis".
●Goals/Objectives:
The program objectives are to provide our concept for Prosthodontics research and to equip students to critically analyze individual research directions.
●Prerequisite Reading
Visit our website for latest published articles.
●Reference Materials
・Designing Clinical Research: Hulley et al., 4th edit, 2013, Lippincott Williams & Wilkins
・McCracken's Removable Partial Prosthodontics: Carr and Brown, 12th edit, 2010, Mosby
・Stewart’s Clinical Removable Partial Prosthodontics: Phoenix, Cagna, DeFreest, 4th Edit, 2008, Quintessence
・See our website for definitive lecture title, schedule and place a few weeks before each lecture.
●Availability in English: Yes
Professor and associate professors of Removable Partial Prosthodontics provides lectures on their specialty research areas in Prosthodontics. Following lecture titles outline the content of this special course; "Two points of research view for tooth loss", "Clinical evaluation of chewing ablity", "Load map to clinical research design", "Biomaterials research in Prosthodontics", "Introduction to stress analysis".
●Goals/Objectives:
The program objectives are to provide our concept for Prosthodontics research and to equip students to critically analyze individual research directions.
●Prerequisite Reading
Visit our website for latest published articles.
●Reference Materials
・Designing Clinical Research: Hulley et al., 4th edit, 2013, Lippincott Williams & Wilkins
・McCracken's Removable Partial Prosthodontics: Carr and Brown, 12th edit, 2010, Mosby
・Stewart’s Clinical Removable Partial Prosthodontics: Phoenix, Cagna, DeFreest, 4th Edit, 2008, Quintessence
・See our website for definitive lecture title, schedule and place a few weeks before each lecture.
●Availability in English: Yes
Special Lecture
“Muscles from prosthodontic aspects”
Lecturer: Prof. Hideharu Hibi (Professor of Depertment of Oral and Maxillofacial Surgery, Nagoya University Graduate School of Medicine)
Date: Feb. 5, 2021 (Fri), 5:30 PM – 7:00 PM using ZOOM
Lecturer: Prof. Hideharu Hibi (Professor of Depertment of Oral and Maxillofacial Surgery, Nagoya University Graduate School of Medicine)
Date: Feb. 5, 2021 (Fri), 5:30 PM – 7:00 PM using ZOOM
“Current situation of digitalization in prosthodontic treatment and its application in super-aged society.”(closed)
Lecturer: Prof. Kazuyoshi Baba (Professor of Depertment of prosthodontics, Showa University)
Date: Feb. 20, 2020 (Thu), 5:00 PM –7:00 PM @ Lecture room No.2(2F Building 7 on the campus map)
“Role of oral and maxillofacial surgery in medical school”(closed)
Lecturer: Prof. Hideharu Hibi (Professor of Depertment of Oral and Maxillofacial Surgery, Nagoya University Graduate School of Medicine)
Date: Jan. 31, 2020 (Fri), 6:00 PM – 7:30 PM @ Lecture room No.2(2F Building 7 on the campus map)
“Quality and quantity of mastication”(closed)
Lecturer: Dr. Kazuhiro Hori (Associate Professor of Division of Comprehensive Prosthodontics, Niigata University Graduate School of Medical and Dental Sciences)
Date: Nov. 29, 2019 (Fri), 5:00 PM – 6:30 PM @ Lecture room No.2(2F Building 7 on the campus map)
Lecturer: Prof. Kazuyoshi Baba (Professor of Depertment of prosthodontics, Showa University)
Date: Feb. 20, 2020 (Thu), 5:00 PM –7:00 PM @ Lecture room No.2(2F Building 7 on the campus map)
“Role of oral and maxillofacial surgery in medical school”(closed)
Lecturer: Prof. Hideharu Hibi (Professor of Depertment of Oral and Maxillofacial Surgery, Nagoya University Graduate School of Medicine)
Date: Jan. 31, 2020 (Fri), 6:00 PM – 7:30 PM @ Lecture room No.2(2F Building 7 on the campus map)
“Quality and quantity of mastication”(closed)
Lecturer: Dr. Kazuhiro Hori (Associate Professor of Division of Comprehensive Prosthodontics, Niigata University Graduate School of Medical and Dental Sciences)
Date: Nov. 29, 2019 (Fri), 5:00 PM – 6:30 PM @ Lecture room No.2(2F Building 7 on the campus map)
Practice
Practices on clinical diagnosis, decision-making, and prosthodontic treatment procedures.
●Available programs:
A yearly removable prosthodontics practice course is provided every month for junior post gradute students. Verifying the schedule at the website is necessary according to the program executed.
●Available programs:
A yearly removable prosthodontics practice course is provided every month for junior post gradute students. Verifying the schedule at the website is necessary according to the program executed.
Lab
Practice on research methods, presentation, and scientific writing by hands-on instructions.
●Available programs:
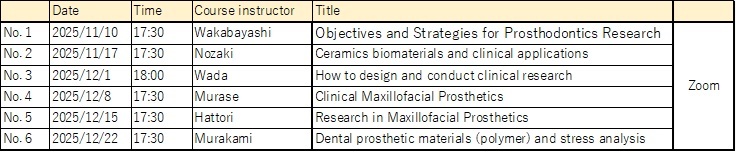
Advanced course of prosthodontics research for postgradute students, six sessions per year. Verifying the schedule at the website is necessary according to the program executed.
●Available programs:
Advanced course of prosthodontics research for postgradute students, six sessions per year. Verifying the schedule at the website is necessary according to the program executed.
Outline of the Doctoral Program, Medical and Dental Sciences Track
See here for details.
Human Resource Development Goals
This course seeks to foster individuals who are thoroughly versed in both the fields of medicine and dentistry and who by creating close links with other fields will play leading roles as researchers within the global arena. It also seeks to foster educators who are capable of designing and implementing effective educational strategies; medical care personnel who are highly specialized, have inquiring minds, and possess a lofty sense of ethics; and opinion leaders who will blaze paths into the future.
Admission Policy
Applicants are required to have broad perspectives, be creative and independent minded, and possess a strong sense of ethics, while being able to logically and accurately articulate their ideas. They must also have a level of English language proficiency sufficient to carry out research work. Furthermore, applicants must have a high degree of scholastic attainment or practical capability in either medicine, dentistry, life sciences and technology, or bioengineering, coupled with a strong will and desire to pursue research in their respective field.
Curriculum Policy
This program creates between fields and disciplines while pursuing a high degree of specialization in areas of research, education, and practice within the realm of medicine and dentistry. To effectively address ethical and social aspects inherent in life sciences, education is advanced with emphasis placed on balance and organic linkage between course work and research training.
Diploma Policy
Degrees are conferred on students who are the course having earned the required credits within the prescribed enrollment period, passed their thesis review and final examination, and fulfilled the following conditions:
-Have produced excellent research results and possess the research ability to contribute to people’s health and wellbeing.
-Possess a high degree of specialization and ethics and the ability to take the lead in advancing creative, trailblazing research.
-Combine multifaceted, specialized expertise related to medical and dental education, and be capable of playing a leadership role within the arena of medicine and dentistry.
-As medical care professional with a high level of expertise, be able to contribute to the advancement of pioneering treatments through clinical research.
-Have produced excellent research results and possess the research ability to contribute to people’s health and wellbeing.
-Possess a high degree of specialization and ethics and the ability to take the lead in advancing creative, trailblazing research.
-Combine multifaceted, specialized expertise related to medical and dental education, and be capable of playing a leadership role within the arena of medicine and dentistry.
-As medical care professional with a high level of expertise, be able to contribute to the advancement of pioneering treatments through clinical research.