Immune checkpoints in T cell-mediated tissue inflammation
PDF Download
- Immune checkpoints in tissue inflammation

Miyuki Azuma
Professor of Molecular Immunology at TMDU
Dr. Azuma completed dental and graduate school at TMDU, where she received her DDS and PhD. She performed postdoctoral research in the Department of Immunology at DNAX Research Institute in Palo Alto, CA, USA and continued her career as an Assistant Professor of Immunology at Juntendo University School of Medicine, and as a Research Associate in the Department of Immunology at National Children’s Medical Research Center in Tokyo. She returned to TMDU as a Professor of Molecular Immunology in 2000.
A: Immune checkpoints help to regulate the immune system. This is important to prevent the development of autoimmunity, which is when the immune system erroneously attacks the body’s own healthy cells instead of invading pathogens or tumors. This regulation is achieved by requiring a second signal for full immune system activation, or by inhibiting activity because the target is recognized as a normal part of the body. In cancer, immune checkpoints are often manipulated to suppress anti-tumor immune responses, allowing the tumor to grow in an unrestricted manner. Additionally, immune checkpoints can also be important in cases of chronic inflammation, in helping to avoid excessive damage to the area surrounding the affected tissue.
A: Masticatory mucosae (the layers of tissues covering the gums, top of the tongue, and hard portion of the roof of the mouth) are specialized oral mucosae for mastication (crushing and digesting foods), as well as protection from environmental damage. Our initial interest in masticatory mucosae arose from histological studies of tissues and cells expressing B7-H1 (also known as PD-L1), which is a ligand (binding partner) for PD-1, an important inhibitory receptor in T cells. We found that masticatory mucosae, but not other oral mucosae or mucosal surfaces of other organs, showed stable expression of B7-H1.
A: We knew that B7-H1 expressed on antigen-presenting cells or tumor cells could interact with PD-1 and inhibit T-cell activation, and that the presence of B7-H1 in tissues could regulate the activation of T cells. However, we did not know how B7-H1 expression was regulated in oral mucosae or how B7-H1 functioned in the oral cavity. The oral mucosae receive external stimuli through the mucosal surface and internal stimuli through immune cells, such as infiltrating T cells and macrophages. Antigen stimulation studies, combined with the use of unique TCR-transgenic mice, allowed us to determine how B7-H1 functions: We learned that keratinocyte/epithelial cell-associated B7-H1 interacts with PD-1 that is expressed on antigen-primed, tissue-infiltrating CD4+ T cells to provide negative regulatory signals.
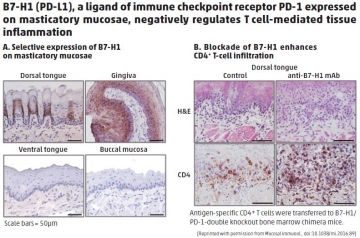
A: The induction of B7-H1 expression in masticatory mucosae appears to be important in the prevention of excess immune responses in chronically inflamed tissue and in homeostasis in the mouth.

