Regenerative Medicine for Inflammatory Bowel Disease
PDF Download
- Regenerative Medicine (PDF: 690KB)

Mamoru Watanabe
Vice President of TMDU
Professor of Gastroenterology and Hepatology
Profile
Dr. Watanabe completed his medical and graduate school at Keio University, where he received his MD and PhD. He performed postdoctoral research at Harvard Medical School in Boston, Massachusetts. He became an Instructor at Keio University Hospital in 1992, then an Associate Professor in 1996. He joined TMDU as a Professor and Chairman of the Department of Gastroenterology and Hepatology in 2000. He became the Vice President of TMDU in 2016.
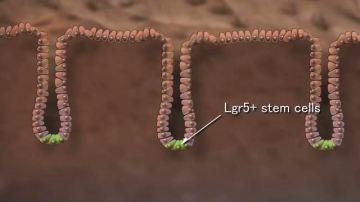
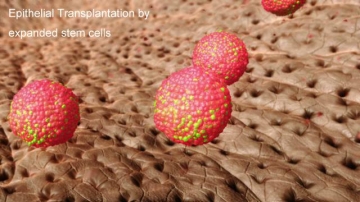
A: We succeeded in establishing our own method (called the TMDU-method) to maintain and efficiently expand mice colonic epithelial stem cells in vitro. By using the TMDU-method, we also succeeded in preparing a large number of colonic epithelial stem cells starting from a single cell, and regenerated damaged colonic mucosa by in vivo transplantation of those ex vivo expanded stem cells. We are now ready to expand human colonic epithelial stem cells in vitro by using endoscopic biopsy specimens as the starting material.
A: “Mucosal healing” (MH) has recently become the most important goal of treatment of inflammatory bowel disease (IBD). However, up to 40% of IBD patients currently fail to achieve MH. Therefore, a new therapeutic approach -- such as regenerative medicine -- is urgently needed. TMDU has long been the world’s leading institution in the treatment of IBD, and enteroscopy techniques. In 2012, we started running the Advanced Clinical Center for Inflammatory Bowel Diseases (ACCIBD), which is dedicated solely to the treatment of IBD. Since then, an increasing number of newly diagnosed IBD patients are rushing to our clinical center. Through the treatment of these patients, we have become quite sure that a new therapeutic approach is needed to improve the prognosis and treatment of refractory patients.
A: We always start thinking from the bedside, not from the bench We know that pluripotent cells, such as iPS cells and ES cells, surely have great scientific, as well as therapeutic, potential. However, to use those cells in clinical applications, we may need to clear various technical as well as ethical problems, which may take many years to solve. In the meantime, why not use adult tissue stem cells? They have low risk of tumorigenicity and do not require time for differentiation. Moreover, we already have a method for preparing the required number of donor stem cells from a small piece of mucosal tissue. This will make it possible to establish and provide stem cell-based regenerative therapy for IBD patients in a minimum period of time.

A: Firstly, it provides an important scientific message that adult somatic stem cells can maintain their identities even in an orthotopic environment. This indicates that those stem cell identities are tightly programmed in the cell - intrinsically - and may not be easily affected by extrinsic signals. Future studies may reveal the mechanism behind how such a tight identity can be maintained in each stem cell. Secondly, from a therapeutic point of view, the data guarantees the therapeutic potential of ex vivo cultured small intestinal stem cells. Thus, the data open a way to use stem cell transplantation to treat refractory small intestinal ulcers that may appear in Crohn’s disease, Behcet’s disease, radiation enteritis or NSAID-induced enteropathy.
A: Currently, we are doing our best to apply our stem cell culture method and transplantation technique to treat refractory ulcers of IBD patients. There still remain plenty of technical problems and regulatory issues that need to be solved, but we now feel quite confident that we are very close to reaching our goal. Also, we are running several basic research projects to find the answer to questions raised in such areas as stem cell biology, mucosal immunology and gastrointestinal oncology. We definitely welcome joint studies with international researchers to share both scientific and therapeutic interests in various areas.
Journal Information
Nat Med., doi: 10.1038/nm.2695
Transplantation of expanded fetal intestinal progenitors contributes to colon regeneration after injury.
Cell Stem Cell., doi: 10.1016/j.stem.2013.09.015.
Small intestinal stem cell identity is maintained with functional Paneth cells in heterotopically grafted epithelium onto the colon,
Genes Dev., doi: 10.1101/gad.245233.114.

