Out with the old, in with the new: Stem cell therapy for inflammatory bowel disease (IBD)
PDF Download
- Stem cell therapy for inflammatory bowel disease (IBD)

Ryuichi Okamoto
Professor of Stem Cell and Regenerative Medicine at TMDU
Dr. Okamoto received his MD and PhD from TMDU in 2004, after which he became a Research Fellow in the Japan Society for the Promotion of Science. In 2007, he became an Associate Professor at TMDU. Since 2013, he has been a Professor at the Center for Stem Cell and Regenerative Medicine at TMDU.
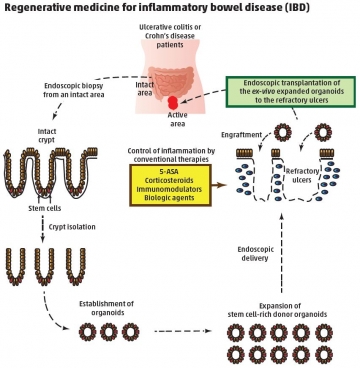
A: Regenerative medicine refers to the repair or replacement of diseased cells, tissues, or organs in order to restore normal function. One way to achieve this is by transplanting stem cells, which are cells that continuously renew themselves and can differentiate into specialized cell types. I work on inflammatory bowel diseases (IBDs) such as Crohn’s disease and ulcerative colitis, which result in damage to the intestinal epithelium (the gut lining). We are looking at ways to remove this damage and regenerate the normal structure through ‘mucosal healing’. We aim to restore the important functions of the gut lining as a mucosal barrier with a role in nutrient absorption, hormone secretion, and immune system regulation. Such treatment contrasts with conventional therapies, which try to reduce inflammation but have limited benefits and are not successful in all patients.
A: Stem cells have been known to exist in the intestinal epithelium since the 1970s. However, the identification of proteins expressed by intestinal stem cells, which can be used as markers to locate the stem cells, was only achieved fairly recently. This has enabled the culture of intestinal stem cells to be refined. They can now be grown in the lab, using suitable growth media and the support of an underlying extracellular matrix, to create a three-dimensional mini-organ, as the TMDU research team headed by Prof. Tetsuya Nakamura reported in an earlier study (Nat. Med., doi: 10.1038/nm.2695). Transplantation of healthy mini-organs to damaged intestines has been achieved in animal models of disease. Stem cells are important to regenerative medicine because they enable lesions to be replaced with healthy tissue.
A: Yes, we are working on a form of therapy for IBD patients who have ulcers that do not respond to current treatments. We are developing a method known as autologous transplantation in which biopsies of healthy areas of the patient’s own intestinal epithelium taken during an endoscopy will be grown in the lab to extract intestinal stem cells. These cells will then be expanded and enriched using our previously established culture techniques. Once we have enough healthy cells for a mini-organ, this can be endoscopically delivered to an ulcerous site in the patient’s gut for repair. The benefits of this include the fact that the mini-organs will not invoke an immune response because they derive from the patient’s own cells, so there should be no barrier to achieving tissue regeneration. However, we first need to maximize the efficiency of this technique, and ensure that the mini-organs can be delivered safely without introducing new problems, such as the development of
tumors.
A: The intestine is made up of multiple cell types, including those of the inner surface of organs and those that line the inside of blood vessels, as well as muscle, nerve, and immune cells. Future work is likely to more accurately reconstruct the three-dimensional culture of mini-organs based on these different cell types. This could eventually lead to the transplantation of the intestine as an entire organ to repair or renew severely damaged lengths of intestine in patients with IBD. Because many of these cell types are involved in disease pathology, stem cells deriving from bone marrow have also been used in the treatment of IBD. So far, this has met with varying levels of success, suggesting further optimization is needed. It is also possible that a combination of cell therapies may improve the clinical outcome. In the future, patients may receive treatment that is better suited to the extent of their disease and the pathologic changes that have occurred.

