Synovial stem cells: Hope for cartilage and meniscus regeneration in osteoarthritis
PDF Download
- Meniscus regeneration

Ichiro Sekiya
Director of the Center for Stem Cell and Regenerative Medicine
Professor of Applied Regenerative Medicine at TMDU
Profile
Dr. Sekiya completed his medical and graduate school at TMDU, where he received his MD and PhD. He performed postdoctoral research in the United States at MCP Hahnemann University and Tulane University. Since 2013, he has been Director of the Center for Stem Cell and Regenerative Medicine and Professor of Applied Regenerative Medicine.
A:Current cartilage repair procedures include bone marrow stimulation to encourage new cartilage to form, but this is limited to small areas and the new cartilage structure may be poor. An alternative involves grafting small plugs of healthy cartilage from low weightbearing areas of joints to damaged regions (mosaicplasty), but this is associated with donor site morbidity. Also, reports on implantation of a patient’s own cartilage cells describe a loss of cartilage cell characteristics. These latter two techniques also involve open surgery, with its associated risks. I have worked with my colleagues at TMDU to devise a minimally invasive method, using a form of keyhole surgery. We harvest the soft tissue of a patient’s joint (synovium), grow the stem cells derived from this, and then transfer them to the damaged area.
A: We enrolled 10 patients in the trial, all with a knee cartilage defect caused by trauma. We removed synovium from each patient and extracted mesenchymal stem cells (MSCs). We cultured these cells in each patient’s own serum, and placed an average of 47 million stem cells in the damaged area using a needle, and kept the patient completely still for 10 minutes. The treatment was effective: MRI analysis showed repair of the area, and replacement cartilage was visible under a microscope. Orthopedic disability was scored and also significantly improved in all patients.
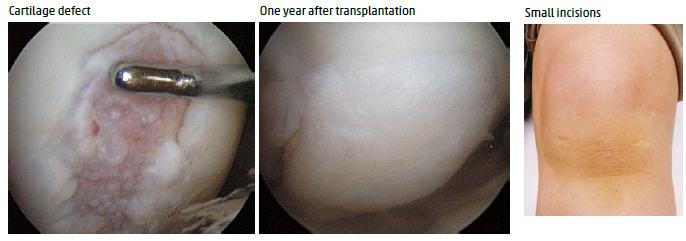
Arthroscopic transplantation of autologous synovial stem cells for cartilage defect
This treatment is effective and possible using small incisions.
A: The meniscus is a crescent-shaped fibrocartilagenous tissue in the knee and has a role in load distribution, stability, and lubrication. Symptomatic degenerative meniscus tears are common, and if surgery is required, arthroscopic partial meniscectomy, instead of meniscus repair, is generally selected due to the poor healing potential of meniscus, although eniscectomy is a cause of osteoarthritis. We performed another clinical study and found that transplantation of synovial MSCs was effective on repaired meniscus with degenerative tears.
A: Knee osteoarthritis, characterized by pathological features including joint space narrowing, is a major public health issue causing chronic pain and disability in the elderly in most developed countries. We performed another clinical study of osteoarthritis in which synovial MSCs were transplanted to defective meniscus and cartilage after the centralization of extruded meniscus. Most patients showed improved clinical outcomes. In some types of osteoarthritis, cartilage can be regenerated with minimally invasive procedures and the transplantation of synovial MSCs.
Journal Information
Clin. Orthop. Relat. Res., doi: 10.1007/s11999-015-4324-8 (2015)

